Balancing Life and Breath: Unraveling the Complexities and History of
Ventilators, From Danger to Lifesaver
Ventilators have been around for decades and have successfully saved the lives of countless patients who were incredibly ill. The significance of ventilators in preserving lives becomes pronounced, particularly in cases where individuals cannot achieve sufficient breathing without external aid. Yet, a sobering truth emerges—a paradox that highlights the delicate balance between medical marvel and potential peril. A paradox that cast a probing spotlight on the intricate web of logistical challenges, controversies, and ethical dilemmas that have interwoven with the ventilator's ascent into medicine. Ventilators are typically considered a last resort in the hierarchy of medical interventions for several reasons.
In this blog post, we will delve into the overarching hazards associated with mechanical ventilation, providing an overview of the impact that the COVID-19 outbreak had on ventilator usage. Additionally, we will explore their efficacy in varying contexts. Take a deep breath as you dive into the captivating, life-saving technology these machines bring into hospitals, and explore past events where ventilators saved thousands.
The Invasive Nature of Ventilators
Ventilators are considered invasive because they involve the insertion of a tube into the patient's airway, which can interfere with the normal functioning of the respiratory system. Using a ventilator comes with several risks for the patient, and certain situations may worsen the patient's condition. For instance, if the patient's condition does not warrant mechanical breathing, a ventilator should avoid being used unless necessary. Furthermore, other procedures, such as a tracheostomy, may need to be performed to insert the breathing tube. Patients on ventilators are also at an increased risk of developing Ventilator-Associated Pneumonia (VAP) due to the presence of the breathing tube, which can introduce bacteria into the airway. Because of these reasons, healthcare providers will first try non-invasive or minimally invasive options to support a patient's breathing before resorting to invasive mechanical ventilation.
Incredible Complexity, both Physically and Through Diagnosis
Ventilators are complex medical devices because they perform precise and critical functions to support a patient's breathing effectively. Several factors contribute to their complexity, including moving parts, intricate system coding, and specialized hardware. Starting with the components,
they are produced with tight tolerancing and high-quality materials. Ventilators must deliver a specific volume of air or oxygen at precise pressures and flow rates to support a patient's respiratory needs. The software, hardware, and other components need to be manufactured with high quality and must be precisely calibrated.
Ventilators also continuously monitor the patient's condition and adjust ventilation accordingly. These live monitoring requirements utilize sensors and real-time data processing, making the software and hardware integration complex. Another complicating issue that comes with developing ventilators is the versatility behind them. Patients that require ventilators all have different conditions and/or disease states. These variables require sophisticated control algorithms and software to adjust the ventilation parameters accordingly.
COVID-19 Muddied "Normal" Treatment for Ventilator Patients
Another intricate part of placing a patient on a ventilator is determining whether they are in such critical condition that it would help or hurt them. Because of the associated risks involving an invasive ventilator procedure, medical professionals carefully diagnose the patient's health before recommending mechanical ventilation.
During the COVID-19 pandemic, this proved incredibly difficult. There were reports of a higher mortality rate among critically ill COVID-19 patients who required mechanical ventilation. Some severe cases of COVID-19, for example, were associated with a hyperinflammatory response, leading to cytokine storms and multi-organ failure, making treatment more challenging. Additionally, some patients had difficulty being weaned off the ventilator once placed on it, leading to prolonged ventilator dependency and associated complications. The virus impeded diagnosis and treatment for patients who required mechanical ventilation, which led to a higher mortality rate in the beginning months of the 2020 outbreak.
However, it is still important to note that while some COVID-19 patients on ventilators faced an increased risk of mortality, mechanical ventilation also played a crucial role in saving lives and providing respiratory support for many critically ill patients. As the understanding of COVID-19 evolved, healthcare providers learned to refine treatment protocols and better manage the use of ventilators, leading to improved outcomes for some patients.
COVID-19 Supply Strain
The COVID-19 pandemic greatly affected how ventilators are regulated, produced, and exported today. The virus resulted in an almost immediate and steep demand increase for ventilators, as patients were entering hospitals with critical breathing conditions. Alongside an over 250% increase in demand for ventilators, the global supply chain was disrupted as travel became highly restricted. Many ventilator components are manufactured and sourced from
different parts of the world, and disruptions in one region affected the overall production and distribution of ventilators.
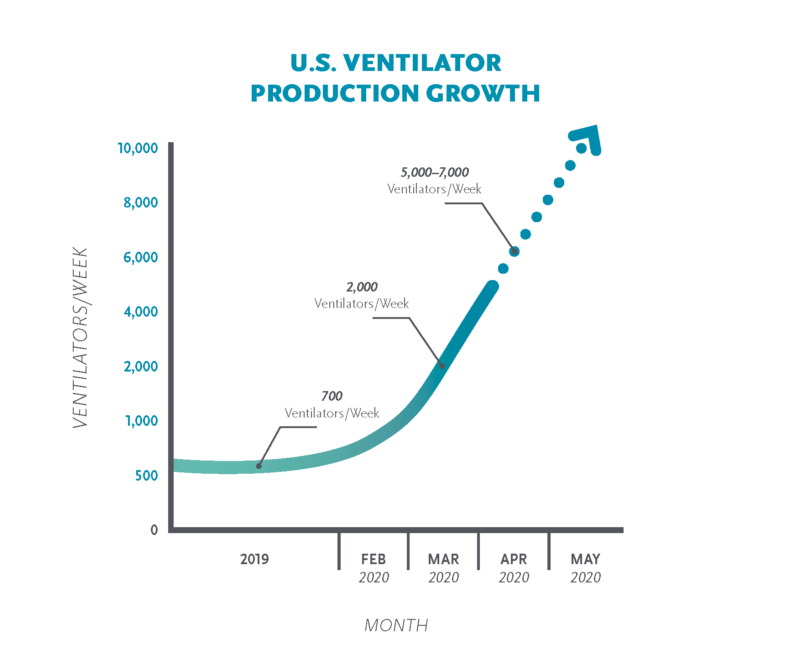
The World Economic Forum constructed the graph above, illustrating the steep and sudden increase in U.S. ventilator production.
Other strains in the medical field during this time included overcrowded hospitals, insufficient medical professionals to treat the ill, and competition for resources; all highlighted the availability issues that ventilators had. COVID-19 proved highly transmissible, leading to a blowout of cases in a short amount of time. In the leading months of the outbreak, hospitals and other medical facilities were unprepared for the testing and treating of the ill.
As a result of the pandemic, governments, and medical institutions have implemented changes in exporting, producing, and regulating ventilators. The pandemic highlighted the need for better preparedness and coordination to ensure an adequate supply of critical medical equipment during public health emergencies. Efforts to strengthen healthcare infrastructure and supply chains continue to be a focus for future readiness.
From Danger to Lifesaver
Despite all of the hardships and risks ventilators carry, they are still incredible pieces of equipment. Overall, ventilators are highly capable, life-saving tools. From short-term usage during surgeries to prolonged support for critically ill patients, these machines can be tailored to provide various ventilation modes, such as pressure-controlled or volume-controlled ventilation, synchronized breaths, and positive end-expiratory pressure (PEEP), all of which contribute to better outcomes for patients. The remarkable capabilities of ventilators have significantly improved patient survival rates, making them indispensable tools in intensive care units and emergency settings where timely and precise respiratory support can be a matter of life and death.
Future steps towards better, risk-minimizing ventilators are constantly being made as this medical marvel continues to save lives.
The ventilator became a medical field success through a careful planning process of design, development, testing, and market research. If you are looking to understand the incredible journey for your idea, be sure to check out The Zewski Report, a Zewski Corporation co-op partner!

